Introduction
Ability Action Australia is a registered NDIS provider of therapeutic, positive behaviour and employment supports across Australia. Our national network of clinics and large pool of mobile clinicians provide participants and their families with fast, life-changing support.
This paper was developed to outline the experiences of our clinicians who faced challenges in tailoring therapies during the restrictions of the COVID-19 pandemic, which limited face-to-face delivery of services. In writing this paper, we unpack these challenges, review international literature, and offer suggestions to map a viable path forward, acknowledging that some pandemic related obstacles will persist for some time.
Adapting to the pandemic
In late March 2020, during Australia’s first wave of COVID-19 infections, the Australian government issued a nonessential business closure direction. This was quickly followed by a stay-at-home direction (see Figure 1). These directions remained in place until 30 May when a ‘stay safe’ direction was issued.
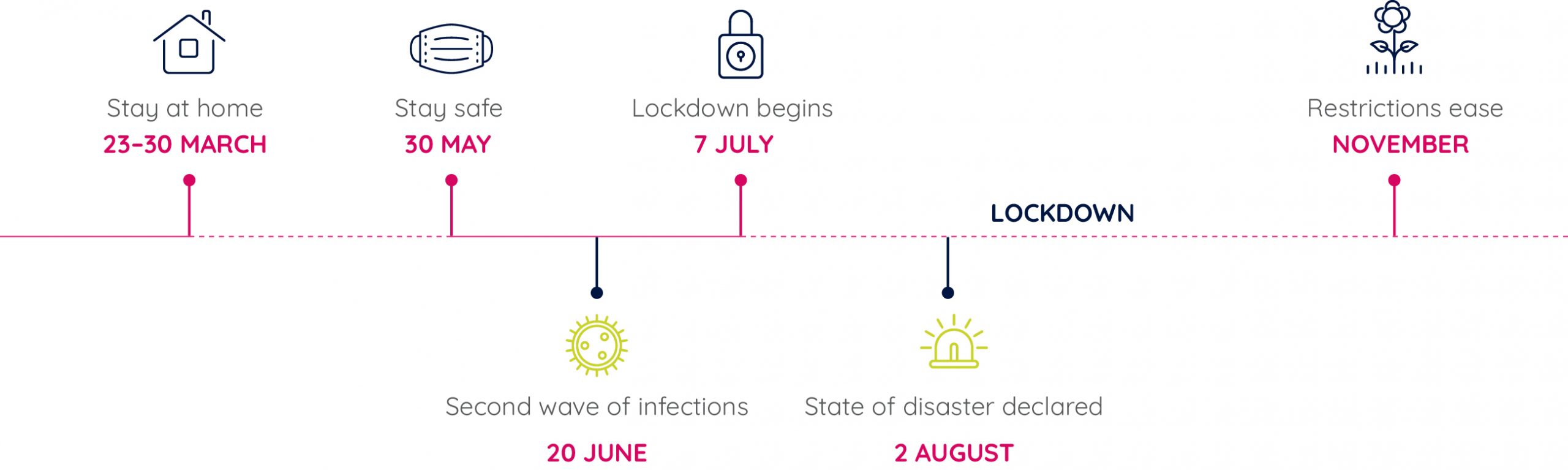
Victoria subsequently experienced a second wave of infections which first became evident on 20 June 2020 as new COVID-19 clusters began to emerge. Restrictions were imposed before a second lockdown period for metropolitan Melbourne began on 7 July, culminating in a state of disaster being declared on 2 August. It was not until November 2020 that restrictions were eased significantly, allowing most businesses to reopen. However, a sense of normality remained elusive for many.
Although Ability Action Australia is now national, at the start of the pandemic it was a young organisation and predominantly Melbourne based. Due to restrictions on face–to–face contact, it was amongst the organisations hardest hit by the restrictions imposed by the Victorian state government. While adapting to their new roles, our team of clinicians also had to be flexible in their approaches to engaging participants, establishing rapport with families, and with service delivery in general. Early in the pandemic, many organisations including in healthcare adopted a positive mindset that things would return to normal before too long. Many people chose to delay treatment, assuming that things would be back to normal soon.
After months of restrictions and delays to normal service provision, however, it became clear that this was a much longer-term issue, and that adapting to this new reality was now urgent so that services essential to the health and wellbeing of many Australians could be delivered. The reality was that many healthcare service providers were struggling to provide the required access to treatment and services to support the wellness of those with long-term disabilities in the face of the COVID-19 restrictions.
Adopting telehealth services
Although telehealth was broadly accepted as a viable mode of delivery for many health services before the pandemic, there were significant delays with both treaters and consumers getting on board. At the height of the restrictions, some face-to-face treatment was still permitted, such as physiotherapy for individuals whose rehabilitation would be set back; however, many clients and treaters either opted out or reduced the frequency of treatment to minimise the risk of infection.
The diversity of services provided by Ability Action Australia as outlined above meant that we could pivot quite easily to telehealth for some types of service provision, such as talking therapies and demonstrating exercises through a screen. Creativity was also applied in certain specialised settings, such as paediatrics where participants were provided with a special ‘therapy box’ containing stickers and fine motor activities to use during telehealth
therapy sessions.
There were other services that proved to be far more challenging to deliver using telehealth, including:
- Therapies for children with autism or developmental delays where focus and concentration might be a challenge
- Activities of daily living (ADL) assessments and home modifications
- Training to improve safety and independence in personal and domestic ADLs
In addition, hands-on therapy such as physiotherapy or swallowing assessments conducted by speech pathologists had to be modified to be suitable for the telehealth environment, and creativity was essential to minimise the loss of therapeutic benefit. An example of a modification was having another person present at the participant end who could work with the participant during the session. This approach also mitigated any risk for participants who may have mobility challenges and therefore may be at risk of falls. This was particularly useful when conducting mobility or safety assessments or training on safe transfers (e.g. in and out of the shower).
Aware of the growing demand for telehealth to deliver occupational therapy services, Occupational Therapy Australia released its ‘Telehealth Guidelines’ in March 2020 (OTA Australia, 2020) to assist members in providing telehealth services. The guidelines aligned with the World Federation of Occupational Therapy’s responsible service provision principles, while minimising professional and clinical risk. The American Occupational Therapy Association released similar guidelines 18 months earlier (AOTA Position Paper, 2018). These guidelines also insisted that telehealth services should continue to be client-centred, evidence-based and meet individual client needs. They provided gold standard guidance regarding risk screening, safety, security, and privacy obligations, and in doing so gave us the confidence to get started with telehealth delivery.
Ability Action Australia continued to adapt to telehealth as well as we could, and even demonstrated innovation in being able to conduct essential home modifications, including a ramp installation, remotely. We also turned to the evidence to explore what others were doing that could be adapted to the needs of our participants in the telehealth setting. The literature provided us with useful learnings from the experience of others, gave us the confidence that we could do it, and also that we could move beyond ‘standard’ to ‘gold standard, tailored telehealth delivery’.
Learnings from international published literature
Cramer et al. (2019), University of California
This paper was published before the pandemic (June, 2019) in a prestigious scientific journal (Journal of the American Medical Association (JAMA)), positioning the University of California as a thought leader in the telerehabilitation space. It adopted a rigorous randomised clinical trial design to evaluate the efficacy of homebased telerehabilitation versus in-clinic therapy for 124 adults after stroke. The study showed comparable efficacy for telerehabilitation relative to traditional in-clinic therapy for improving motor status (substantial gains in arm motor function were demonstrated across both modes of delivery) and patient knowledge.
This paper is one of the first to demonstrate that telehealth works effectively for basic neurorehabilitation therapies post-stroke. Findings were also extrapolated to suggest that telerehabilitation has the potential to increase access to rehabilitation therapies on a large scale.
Khan et al. (2021), New York University
Recognising the urgent need for tele-psychiatry in the face of the pandemic, this article described the development of an open access national online curriculum for medical education on the topic of paediatric tele-psychiatry. As suggested by the authors, tele-psychiatry offers the potential for convenient, cost-effective, and high quality care. It also has the potential to greatly improve access to paediatric psychiatric care, but training of clinicians is required to ensure the delivery option is incorporated into standard practice on a needs basis, and that high quality care standards are maintained for this mode of delivery.
Importantly, several studies in general and child psychiatry have demonstrated that clinical care delivered using tele-psychiatry is equivalent, and in some cases superior to, in-person care. Evidence has also shown that telepsychiatry can also reduce stigma, especially for vulnerable populations including children, veterans, those in rural or remote areas, individuals serving time in prison and non-English speakers.
The curriculum development adhered to a robust and well-accepted framework that conducted a needs assessment, developed content to address goals and measurable objectives, and incorporated expert review and refinement. Importantly, the online format allows for ongoing revision as the tele-psychiatry landscape is further finetuned.
Sharma et al. (2020), University of Washington, Seattle Children’s hospital
This article describes the transitioning of an acute outpatient child and adolescent psychiatry service to a homebased tele-mental health (TMH) service/virtual clinic during the COVID-19 pandemic. Within a six-week period, this service pivoted to providing 92% of sessions remotely notwithstanding an IT platform failure likely due to excessive use. The paper provides a useful roadmap for rapidly establishing a service that was entirely dependent on telemedicine/telerehabilitation delivery.
The majority of challenges were addressed by using clear protocols (including ensuring all staff were adequately trained) and risk screening/mitigation strategies (modified consent procedures), and were also greatly reliant on increased administrative support with scheduling and billing, and IT assistance. Importantly, existing TMH guidelines and experience with telehealth delivery were used to ensure that the TMH service provision was safe, secure as well as effective and that it was able to effectively monitor safety in crisis situations with especially vulnerable individuals.
Yosef et al. (2019), Hebrew University of Jerusalem, Israel
This pilot study provided preliminary evidence that telehealth can be successfully used for functional goal-oriented activities of daily living (ADL) therapy with adults with an acquired brain injury (ABI).
The intervention provided functional ADL assessment and cognitive re-education over 15 telehealth sessions over a three-month period (1-2 times per week) for a small group of five adults in the chronic stage after ABI (6-10 months post), who were living within the community. Three of five functional goals determined by the Canadian Occupational Performance Measure were the focus of the intervention which used a performance-based approach.
The pilot showed preliminary evidence of efficacy with improvement in the primary outcome of personal functional goals. It also demonstrated feasibility in using telehealth technology and high participant satisfaction. Recommendations from the pilot included that there needs to be appropriate guidance and adequate technical support when delivering interventions via telehealth.
Buckingham et al. (2022), Universities of Plymouth and Southampton, UK
This group of academics and health professionals codeveloped and evaluated a telerehab toolkit that has been disseminated widely and made freely available online for practitioners, patients and carers. Development was informed by current evidence, findings from an online survey, service evaluation and focus group discussions with key stakeholders.
Though the primary context of the toolkit is remote physical assessments for those with physical disabilities and movement impairments, it also contains information on technology, digital skills, remote assessment tools, information governance, and safety for telerehabilitation. Resources are targeted toward patients as well as practitioners and include tips from clinicians and patients, step-by-step guides and checklists, and videos. Links to evidence are also provided.
Conclusion and what’s next?
Collectively, the studies had useful learnings and gave us confidence that within the restraints of the pandemic and restrictions on face-to-face interactions we could continue to deliver services to our participants, while maintaining effectiveness and quality of service delivery, and not creating risks to safety or privacy.
However, it was important to reflect on the need to support participants with accessing therapy via the technology platforms, which was also a common frustration within many of the study cohorts. It is not sustainable for clinicians to spend 10 to 15 minutes assisting their participants to log on and be able to navigate the technology. Along with tip sheets, it is important to provide an administrative support who can check that, from a participant’s perspective, everything is working prior to the appointment time, to avoid wasting valuable treatment time in trouble-shooting.
For Ability Action Australia and our participants, telehealth provided a useful alternative to our traditional modes of service delivery. All parties have built confidence and familiarity in telehealth, and it is here to stay. Telehealth provides an additional option in support of participant choice and control over how services are delivered. It remains particularly useful in regional and remote areas, where there may be no relevant therapist in an area. It is also a useful option during times of ill-health when a participant is unable to travel to a clinic, or would prefer to limit exposure to others.
References
American Occupational Therapy Association. Telehealth in occupational therapy. American Journal of Occupational Therapy 2018 72 (Suppl. 2), 7212410059. https://doi.org/10.5014/ajot.2018.72S219
Buckingham S, Anil K, Demain S, et al. Telerehabilitation for people with physical disabilities and movement impairment: development and evaluation of an online toolkit for practitioners and patients. Disability and Rehabilitation 2022. DOI: 10.1080/09638288.2022.2074549
Cramer SC, Dodakian L, Le V, et al. Efficacy of Home-Based Telerehabilitation vs In-Clinic Therapy for Adults After Stroke. Journal American Medical Association (JAMA) Neurology 2019 76(9) 1079 – 1087
Khan S, Myers K, Busch B, et al. A National Pediatric Telepsychiatry Curriculum for Graduate Medical Education and Continuing Medical Education. Journal of Child and Adolescent Psychopharmacology 2021
Occupational Therapy Australia (OTA) Telehealth Guidelines. [Last updated 20 March, 2020]. Accessed from: https://otaus.com.au/publicassets/553c6eae-ad6c-ea11-9404-005056be13b5/OTA%20Telehealth%20Guidelines%202020.pdf
Sharma A, Sasser T, Schoenfelder G, et al. Implementation of Home-Based Telemental Health in a Large Child Psychiatry Department During the COVID-19 Crisis. Journal of Child and Adolescent Psychopharmacology 2020 30 (7) 404 – 413
Yosef AB, Jacobs JM, Shenkar S, et al. Activity Performance, Participation, and Quality of Life Among Adults in the Chronic Stage After Acquired Brain Injury – The Feasibility of an Occupation-Based Telerehabilitation Intervention. Frontiers in Neurology 2019 10: 1247
Click here to download this document as a PDF.

